With any treatment, including treatment for opioid addiction, certain principles apply that greatly improve response. These include early detection (screening) and early intervention; comprehensive care, which involves providing treatments that bridge psychosocial, recovery-based, and biological care; continuous care, which means not stopping and having to restart treatment; and a true partnership with the patient (and family), often called “shared decision making” because we all are more apt to do what we decide to do rather than what we are told to do. Another principle, which is too often overlooked, is detection and treatment of any co-occurring mental or general medical condition. No one recovers from an opioid use disorder unless his or her other ailments are identified and treated.
Treatments for opioid use disorder fall into two main categories: medications and psychosocial approaches. Treatments work, but not for everyone.
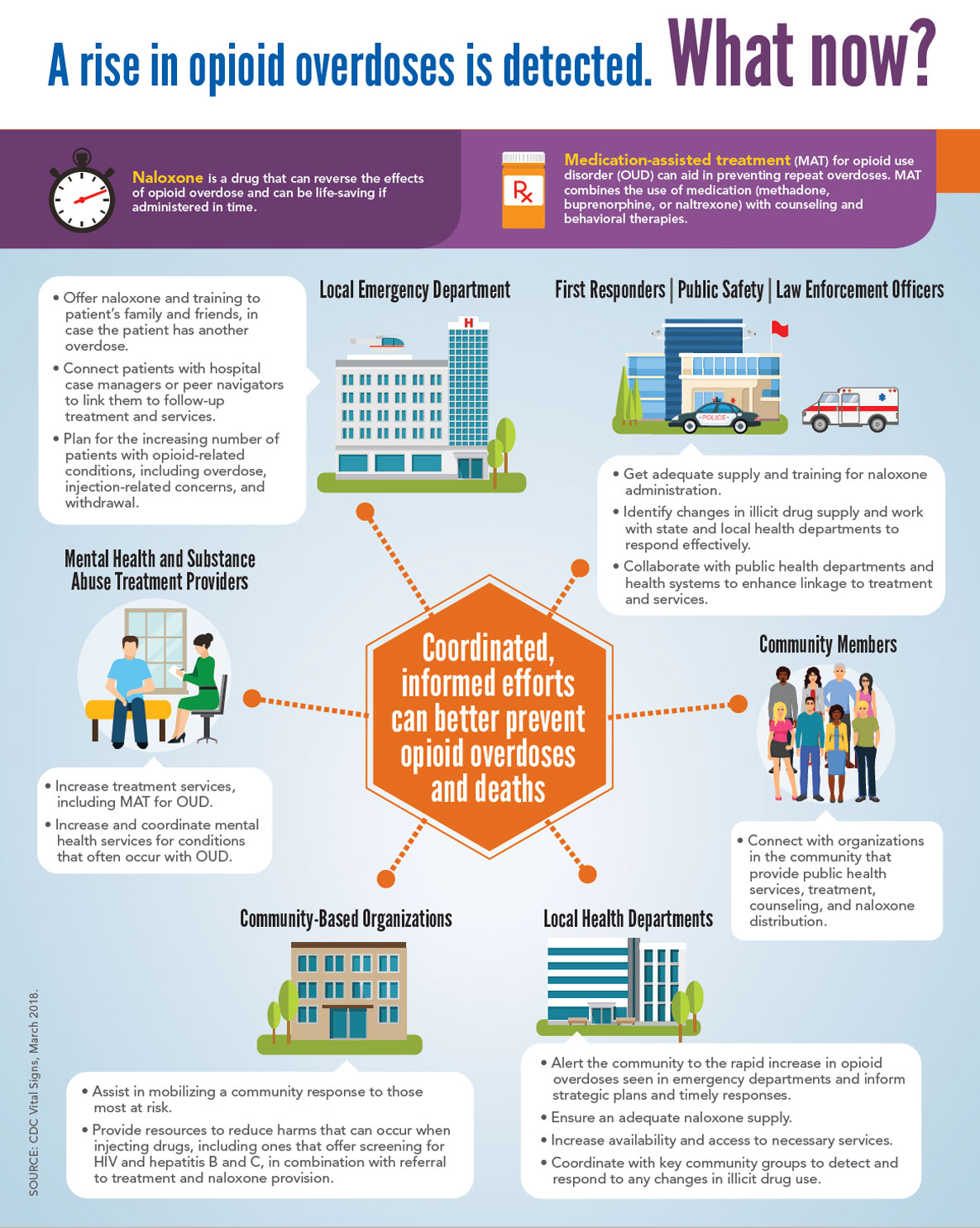
Medication-assisted treatment (MAT)
Opioid agonists are drugs that bind to opioid receptors and produce similar effects, such as pain relief. Methadone is an opioid agonist, and buprenorphine is an opioid partial agonist. Both are used to treat opioid use disorder. Methadone was introduced by Doyle and Nyswander in the early 1960s as a maintenance treatment; it has established effectiveness, especially when combined with counseling and medical and social services. In 2002
Principles that greatly improve response to treatment:
- Early detection (screening) and early intervention
- Comprehensive care, which involves providing treatments that bridge psychosocial, recovery- based, and biological care
- Continuous care
- Shared decision making with patient and family
Detection and treatment of any co-occurring mental or general medical condition
Buprenorphine was legalized and made available in the United States. It is effective for people with mild-moderate opioid dependence, safer in overdose than methadone, and a 30-day supply can be dispensed from a physician’s office. Far too few physicians have obtained the special training and Drug Enforcement Administration designation required to prescribe buprenorphine, which has created a barrier to wider use of this treatment, and even among those who have done so, it appears that few prescribe the drug. Both methadone and buprenorphine carry the unfortunate stigma of using a drug to treat a drug problem.
Opioid antagonists are also used to treat opioid use disorder. The most common are naloxone, naltrexone, and extended-release naltrexone (Vivitrol). Naloxone, which can be given intravenously, injected into a muscle, or sprayed into the nose, is foremost a lifesaver, because it can immediately reverse the often fatal respiratory effects of an opioid overdose. In its various forms, it is becoming ubiquitous among emergency responders, individuals who use opioids, and their families and friends. Naltrexone, a variant of naloxone in pill form, has been used to reduce cravings and the rewarding effects of alcohol and other drugs, including opioids. Vivitrol, which is a monthly intramuscular injection, was first developed for reducing rates of drinking among persons with alcohol dependence and may hold promise for treating opioid use disorder. Early results for Vivitrol among individuals with a history of opioid use disorder released from correctional settings are promising.
Other preparations have been used in the MAT of opioid use disorder. One is acamprosate, but there has been limited study of its effectiveness to date. It may modulate brain glutamate receptors, thereby diminishing withdrawal, a trigger for relapse. Another is NAC (N-acetylcysteine), which is available over the counter from vitamin markets and online, and scientific study is under way. NAC also has effects on glutamate (and dopamine) transmission in the brain and may quiet systemic inflammation; it has been used to treat cannabis dependence.
Psychedelic drugs (especially psilocybin) and cannabis are also being considered to treat opioid use disorder. A “trip” can change a person and can alter dependence on opioids or other substances, and we should not dismiss this approach until more is known. Cannabis may reduce use of opioids as an analgesic, and studies are under way to assess the effectiveness of cannabis in this regard.
Psychosocial interventions
Psychosocial interventions can be effective in treating opioid use disorder. Good outcomes can be achieved by participation in 12-step recovery programs, including Narcotics Anonymous (NA), and related support and educational groups for families with a loved one in recovery. A common misconception is that 12-step programs require a religious orientation or a specific faith. Instead, an individual’s sense of a higher power, however ill defined, resonates with 12-step programs and provides an anchor on the road of recovery. There is considerable controversy regarding the percentage of NA participants who remain clean and sober because NA’s requirement of anonymity limits research studies.
Motivational interviewing (or motivational enhancement) is a counseling approach that has been successful in helping people recover from addictive disorders. People take opioids for a reason and continue for the same or other reasons (such as to deter withdrawal symptoms). Thus the work of treatment begins with assessing a person’s readiness to change and helping tilt that readiness to action. Motivational interviewing (or enhancement) is a skill that clinicians, including primary care physicians, can learn and employ briefly to help someone with drug dependence take steps to quit or reduce harm.
Another counseling approach is cognitive-behavioral therapy (CBT), which is based on the central premise that how we think affects how we feel and behave. For habit disorders, such as opioid addiction, recognizing triggers, developing alternative and positive thoughts, and avoiding high-risk situations can be lifesaving. CBT is time limited and can be conducted in groups as well as individually. Research has been limited because of the difficulties inherent in studying this intervention among opioid users.
Group therapy, especially relapse prevention groups, is another approach to addiction treatment. The power of a group is perhaps nowhere as plain as among individuals with addictive disorders, including opioid addiction. In relapse prevention groups, members learn to understand triggers and the behaviors to avoid them, and they experience group support.